World AIDS Day: HIV & The Truth About PrEP
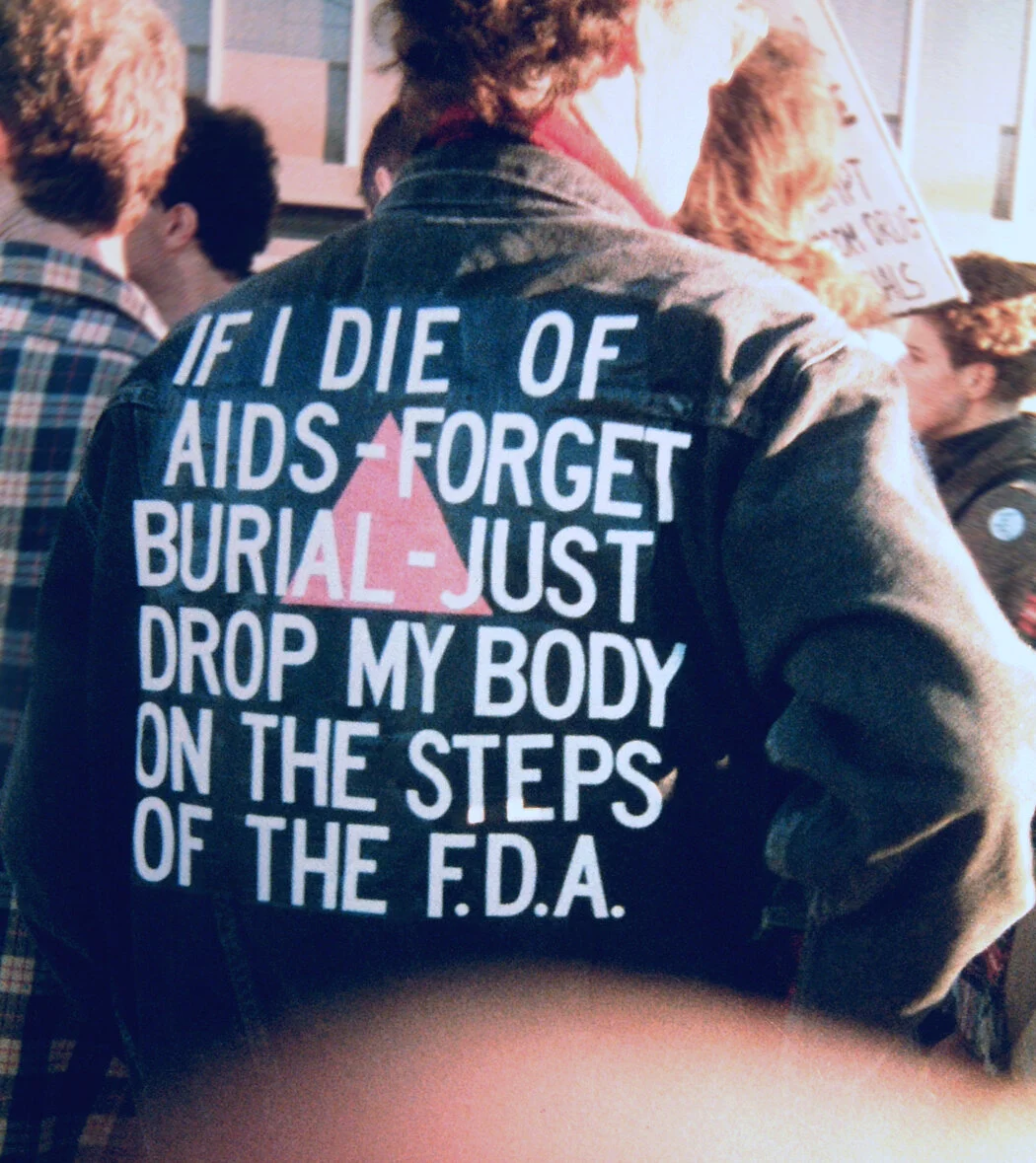
Today is World AIDS Day. Here’s a brief historical look at the significance of this day, courtesy of Matt Bernstein. We recommend further educating yourself if you are not so on this issue.
During your TV commercial breaks you may have seen or heard a drug ad about PrEP, and although there are advertisements about PrEP, many people are unaware this drug exists.
So, what exactly is PrEP?
Well, the ad usually goes a little something like this, “PrEP is a biomedical intervention indicated to reduce the risk of sexually acquired HIV-1 in adults and adolescents less than or equal to 35 kilograms who are at risk for HIV when used in combination with safer sex practices.”
Safe sex practices with condoms combined with PrEP can substantially reduce the risk of HIV infection. In the event resistance is present in the HIV positive partner it is still possible to transmit the HIV infection. Truvada for PrEP comes in a tablet form and taken once daily. It also requires monitoring for HIV negative results at 30 and 90 days upon intitation of treatment. It’s manufactured by Gilead sciences, and has been approved since July of 2012.
There are also several compelling research trials that demonstrate the efficacy of reducing transmission in individuals who are HIV negative. The iPrEX study researched PrEP in negative men and transgendered women who have sex with men, and the results concluded that PrEP reduced the risk of acquisition by 90 percent. The Partners PrEP study concluded a 92 percent reduction in risk of transmission of HIV-1 infection. These results were seen after the studies for those who had detectable concentrations of TruvadaÆ in their bloodstream.
“The Centers for Disease Control and The US Public Health Service recommends that daily oral PrEP should be considered for HIV uninfected patients with any of the following indications:
Anyone who is in an ongoing sexual relationship with and HIV-infected partner
A gay or bisexual man who has had sex without a condom or has been diagnosed with a sexually transmitted infection within the past six months, and is not in a mutually monogamous relationship with a partner who recently test negative
A heterosexual man or woman who does not always use condoms when having sex with partners known to be at risk for HIV, and is not in a mutually monogamous relationship with a partner who recently test HIV negative.
Anyone who has within the past six months injected illicit drugs and shared equipment or been in a treatment program for injection drug use.”
How do I access PrEP?
Although, PrEP has been on the market for 7 years, there are still barriers to obtaining this medication. Truvada is available only by prescription. It can be prescribed by a licensed practitioner who has an established patient relationship (i.e. primary care provider, gynecologist). Clinicians that are not educated on how to prescribe PrEP for prevention which can be a barrier to access. However, there are prescribing guidelines established by CDC and the US Public Health Service to support clinicians needing more education on prescribing PrEP.
Truvada’s cost is also a barrier with a price tag of over $2000.00 for a month supply. Most public health insurances such as Medicaid and Medicare will cover Truvada for PrEP. Private insurers will more likely have this medication on the highest tier of the formulary, making it very expensive or totally eliminating coverage of the medication. The manufacturer, Gilead Sciences, also has a prescription assistance program for those without any coverage. Also contact your local or state health department to inquire if they provide prescription drug assistance for PrEP.
The United States now has a plan to end the HIV epidemic by 2030. The plan also involves a major push toward providing access to PrEP in order to advance toward this goal in 48 counties, rural communities in 7 states with disproportionate occurrence of HIV, Washington D.C., and San Juan, Puerto Rico. It is actually one of the health outcomes the Trump Administration has promised to deliver on during his presidency in his February 2019 state of the union address. President Trump has announced over 221 million dollars will be appropriated to make this happen by 2030. On June 4th the Center for Strategic and International Studies held a discussion with Dr. Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases, and Dr. Robert Redfield, Director of the U.S. Centers for Disease Control and Prevention, about the 10 year strategy on how the US will execute the end the epidemic plan by 2030 with all of the current challenges “around financing, coordination, outreach to marginalized communities, and addressing a variety of implementation challenges.”
So why now? HIV is a preventable disease, and now a chronic condition. It’s approximated that there are over 39,000 new infections every year with 20 percent of the population still undiagnosed despite the advancement in HIV science. I would like to be optimistic this goal is achievable for the U.S. There are social determinants of health such as stigma, health literacy deficiencies, and the lack of access to affordable housing are real, which makes this goal very challenging. I think Dr. Robert Redfield said it best “stigma is the enemy of public health,” and that “HIV is a medical condition not a moral failing.” Just maybe ending HIV could happen, and mark one of the greatest accomplishments in modern day medicine this century.